What is this?
Placenta praevia percreta
The image is an intraoperative picture taken of a pregnant uterus at 35+5 weeks gestation. In the lower section, you can see diffuse vasculature and the bulge of a placenta praevia. The engorged venous plexuses on each side are a normal pregnancy finding, especially when the uterus is exteriorised.
Note: explicit patient consent obtained for publication of images.
Antenatal period
The patient had 4 previous caesarean sections and was transferred from a regional hospital due to the complex pregnancy and surgical management required.
Images below include abdominal ultrasound, transvaginal ultrasound and MRI to try and determine whether the placenta praevia had invaded through the myometrium and/or into surrounding structures such as the bladder or parametrial tissue.
Ultrasound is usually the preferred imaging option, but MRI can on occasion provide additional information to help with planning delivery.
Image shows intense vascular network - placental body to the left, bladder to the right.
Image demonstrates placental body on the left and possible invasion through myometrium into bladder serosa on the right.
Transvaginal ultrasound scan. Placenta on the left, with high level doppler signal indicating a large plexus of vasculature below placental implantation, at the level of the bladder reflection, down to the cervix.
Sagittal plane MRI showing placenta praevia with a suspicion of percreta, but the imaging was unable to confirm or refute bladder invasion.
Final MFM image report
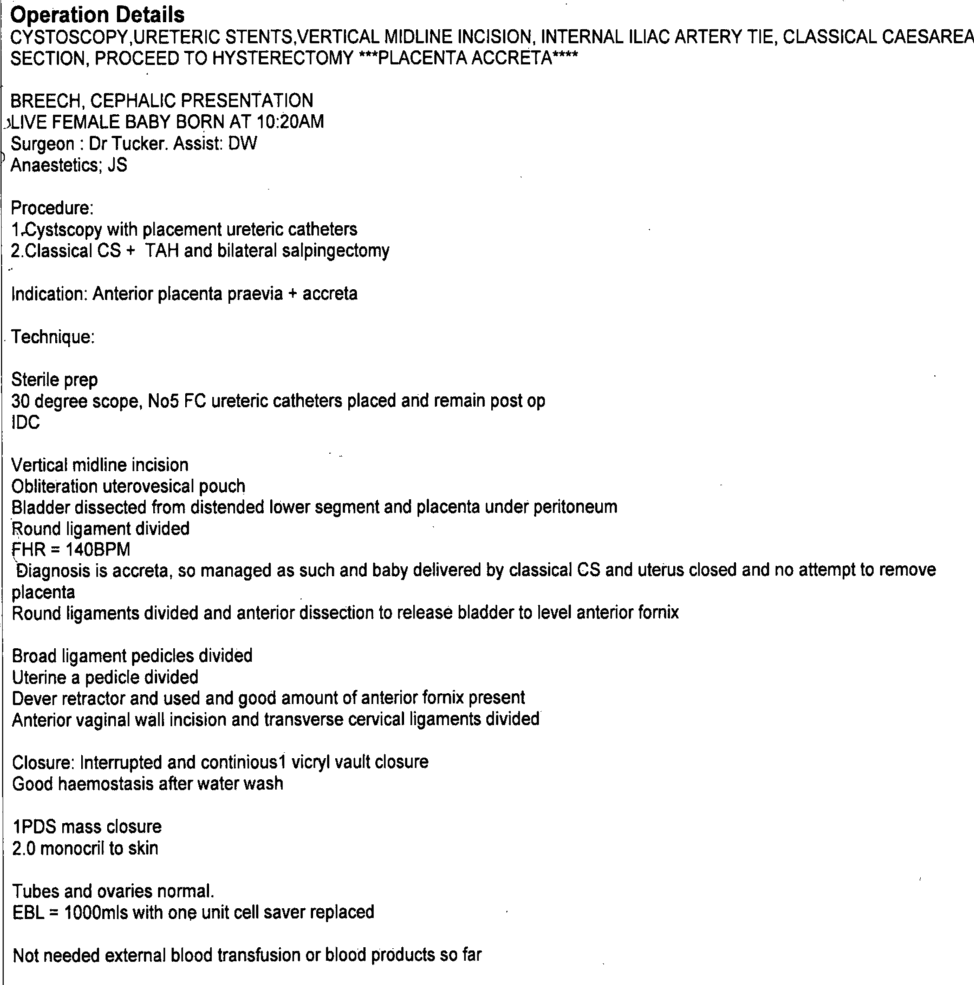
The patient underwent a planned caesarean section as per plan in MFM report above. Typically, blood loss during delivery with suspected placenta accreta is at least 1 litre with 2-3 litres not uncommon. Packed red cells were cross-matched as a precaution. Cell salvage was used to recirculate the patient’s blood back into her circulation.
Anaesthesia anxiously awaiting the incision into the uterus!
Left image: baby delivered, uterine incision closed, placenta seen below and left in situ.
Right image: hysterectomy completed and vaginal vault being sutured.
The mother had an uncomplicated recovery and was discharged to local accommodation on day 6 post-op. Shortly after both mother and baby returned to their local hospital for the remainder of neonatal care.
Day 0 on the Special Care Nursery
Placenta accreta spectrum (PAS) disorders describe different grades of abnormal attachments of the placenta to the uterine wall.
It results from a failure of normal decidualisation in an area of a previous uterine scar.
In placenta creta villous tissue adheres directly to the myometrium without invading the uterine wall.
In placenta increta the villous tissue invades the myometrium.
In placenta percreta the villous tissue invades the entire thickness of myometrium including the uterine serosa.
The different grades of placenta accreta spectrum disorders may coexist within the same placenta, as illustrated above.
Final histopathology report.
More interesting placental pictures in this social media post.
DT